|
Download Adobe Reader
 Resize font: Resize font:
Paroxetine
2018, University of California, Merced, Pyran's review: "Paroxetine 40 mg, 30 mg, 20 mg, 10 mg. Cheap Paroxetine online in USA.". Its purpose was to increase the likelihood that decision making as it relates to diagnostic error and over- the correct diagnosis appeared on the list of differential confidence buy discount paroxetine 10mg, which is expanded upon by their colleagues generic paroxetine 20 mg otc. Pat Croskerry and Geoff Norman ingly apt (and offered free of charge by Missouri Regional review 2 modes of clinical reasoning in an effort to better Medical Program), the system produced many astonishing understand the processes underlying overconfidence. Wears highlight gaps in garding “tough” cases, but no rush to employment or major knowledge about the nature of diagnostic problems, empha- changes in mortality rates. Clearly, many experts are con- these present efforts to study diagnostic decision making cerned about these processes. In closing, I applaud espe- professional or lay reader who thinks it is easy to bring cially the suggestions to systematize the incorporation of the medical decision making closer to the ideal. Schiff in lems likely will not get better until the average day does the fourth commentary, “Learning and feedback are insep- confront us with our errors. This analytic review concerns the exceptions: the times when these cognitive processes fail and the final diagnosis is missed or wrong. We argue that physicians in general underappreciate the likelihood that their diagnoses are wrong and that this tendency to overconfidence is related to both intrinsic and systemically reinforced factors. We present a comprehensive review of the available literature and current thinking related to these issues. The review covers the incidence and impact of diagnostic error, data on physician overconfidence as a contributing cause of errors, strategies to improve the accuracy of diagnostic decision making, and recommendations for future research. In that survey, 35% 1 —Fran Lowry experienced a medical mistake in the past 5 years involving 2 themselves, their family, or friends; half of the mistakes were Mongerson describes in poignant detail the impact of a described as diagnostic errors. Interestingly, 55% of respondents listed veys of patients have shown that patients and their physi- misdiagnosis as the greatest concern when seeing a physician cians perceive that medical errors in general, and diagnostic in the outpatient setting, while 23% listed it as the error of most errors in particular, are common and of concern. Concerns about medical errors stance, Blendon and colleagues surveyed patients and phy- also were reported by 38% of patients who had recently visited sicians on the extent to which they or a member of their an emergency department; of these, the most common worry family had experienced medical errors, defined as mistakes 5 was misdiagnosis (22%). For this reason, we have Statement of author disclosures: Please see the Author Disclosures reviewed the scientific literature on the incidence and im- section at the end of this article. Department of Health Services Administration, School of Health Profes- In the latter portion of this article we review the literature on sions, University of Alabama at Birmingham, 1675 University Boulevard, Room 544, Birmingham, Alabama 35294-3361. In 1 such generally lowest for the 2 perceptual specialties, radiology study, the pathology department at the Johns Hopkins Hos- and pathology, which rely heavily on visual interpretation. A similar study at ology and anatomic pathology probably range from 2% to Hershey Medical Center in Pennsylvania identified a 5. The typically low error rates in these specialties should not be expected in those practices in tissues from the female reproductive tract and 10% in and institutions that allow x-rays to be read by frontline cancer patients. Certain tissues are notoriously difficult; for clinicians who are not trained radiologists. For example, in example, discordance rates range from 20% to 25% for 21,22 a study of x-rays interpreted by emergency department lymphomas and sarcomas. A study of admissions to dance rate in practice seems to be 5% in most British hospitals reported that 6% of the admitting diag- 25,26 cases. The emergency department requires Mammography has attracted the most attention in re- complex decision making in settings of above-average un- gard to diagnostic error in radiology. The rate of diagnostic error in this arena variability from one radiologist to another in the ability to 14,15 ranges from 0. A recent study of breast cancer found that the nostic error in clinical medicine was approximately 15%. In diagnosis was inappropriately delayed in 9%, and a third this section, we review data from a wide variety of sources 29 of these reflected misreading of the mammogram. Several studies have ex- frequently recommending biopsies for what turn out to be amined changes in diagnosis after a second opinion. Given the differences regarding insurance 17 coverage and the medical malpractice systems between and associates, using telemedicine consultations with spe- cialists in a variety of fields, found a 5% change in diagno- the United States and the United Kingdom, it is not sis. There is a wealth of information in the perceptual surprising that women in the United States are twice as specialties using second opinions to judge the rate of diag- likely as women in the United Kingdom to have a neg- 30 nostic error. It is important to emphasize that only a fraction of the 18,27,31–46 studies that have measured the rate of diagnos- discordance in these studies was found to cause harm. An unsettling consistency emerges: the frequency of diagnostic error is disappoint- Dermatology. For exam- tions and disorders where rapid and accurate diagnosis is ple, in a study of 5,136 biopsies, a major change in diag- essential, such as myocardial infarction, pulmonary em- nosis was encountered in 11% on second review. Of6 at ien t w ho died o fp ulm o n ar y em b o li m , he diagn o s i w as n o t us ect ed clin ically in L eder le et al( up ur ed ao r ic an eur ys m eview o fallcas es at a in gle m edicalcen t er o ver a yr er io d. Of2 cas es in vo lvin g ab do m in alan eur ys m s vo n o do li ch et al diagn o s i o fr up ur ed an eur ys m w as in iially m i ed in in at ien t es en t in g w ih ches ain , ( diagn o s i o fdi ect in g an eur ys m o ft he p o xim alao r a w as m i ed in o fcas es E dlo w Sub ar achn o id hem o r hage Up dat ed eview o fp ub li hed udies o n ub ar achn o id hem o r hage: ar e m i diagn o s ed o n in iialevaluat io n B ur o n et al( an cer det ect io n ut o p y s udy at a in gle ho s ial o ft he 2 m align an t n eo p las m s fo un d at aut o p y, w er e eiher m i diagn o s ed o r un diagn o s ed, an d in o ft he cas es he caus e o fdeat h w as judged o b e r elat ed o he can cer B eam et al( eas can cer accr edied cen t er agr eed o eview m am m o gr am s o f7 w o m en , o fw ho m had b r eas can cer he can cer w o uld have b een m i ed in M cG in n i et al( elan o m a Seco n d eview o f5 b io p y s am p les diagn o s i chan ged in fo m b en ign o m align an t fo m m align an t o b en ign , an d had a chan ge in um o r gr ade) Per li i o lar di o r der The in iialdiagn o s i w as w r o n g in o fp at ien t w ih b i o lar di o r der an d delays in es ab li hin g he co r ect diagn o s i w er e co m m o n G affet al( en dicii et o s ect ive s udy at ho s ial o fp at ien t w ih ab do m in alp ain an d o p er at io n s fo r ap en dicii Of1 p at ien t w ho had ur ger y, her e w as n o ap en dicii in o f9 at ien t w ih a fin aldiagn o s i o f ap en dicii he diagn o s i w as m i ed o r w r o n g in R aab et al( an cer at ho lo gy The feq uen cy o fer o r in diagn o s in g can cer w as m eas ur ed at ho s ial o ver a yr er io d. The autopsy has been described as “the What Percentage of Adverse Events is 47 most powerful tool in the history of medicine” and the Attributable to Diagnostic Errors and What “gold standard” for detecting diagnostic errors. Richard Percentage of Diagnostic Errors Leads to Cabot correlated case records with autopsy findings in Adverse Events? In the Harvard Medical Practice Study of tween clinical and autopsy diagnoses were found in a 30,195 hospital records, diagnostic errors accounted for more recent study of geriatric patients in the Nether- 58,59 50 17% of adverse events. On average, 10% of autopsies revealed that the study of 15,000 records from Colorado and Utah reported clinical diagnosis was wrong, and 25% revealed a new that diagnostic errors contributed to 6.
Facial bone imaging using cephalography is mainly used as part of orthodontic assessment buy 10 mg paroxetine free shipping. Although analogue (film based) imaging is still widespread buy discount paroxetine 40 mg online, digital systems are increasingly widespread and have become predominant in some developed countries. A recent review of the literature has confirmed this, at least for the simple radiographic techniques [4]. These figures must be viewed with caution; dosimetry performed as part of scientific studies presents results from modern equipment in carefully controlled situations. Where large studies have been performed on equipment in primary dental care, a wide range of radiation doses is revealed with an elongated tail at the high dose end [3, 5–12]. Payment, whether by the patient directly, through private insurance or public health service systems, is a motivation for intervention. While evidence for this is often anecdotal, recent research has shown the impact on prescription of radiography when a public health service payment system changed [13]. There are other, more subtle, pressures on dentists to use radiography; in particular, there can be fears of missing something and facing consequent medico-legal problems [14]. Dentists are strongly influenced by peer pressure to use X rays, patient expectations and by the teaching received in undergraduate training. As with medical radiology generally, there have been efforts to introduce guidelines (referral criteria) on prescription of diagnostic dental X ray examinations, for example, in Europe and in the United States of America [14, 15]. The quality of such guidelines varies, ranging from expert opinion of a small self-selected panel of individuals, through consensus statements of larger groups, to evidence based guidelines produced using robust methodologies. Guidelines are useless if they are not adopted and incorporated into the education of clinicians (undergraduate and continuing professional education). There is a paucity of current evidence for awareness of and adherence to published referral criteria. Intraoral radiography for detection of dental caries (decay) is the most commonly performed X ray examination in dentistry, but intervals between examinations should be matched to clinical criteria of risk of disease [15, 18]. There is a perception, sometimes implicit in manufacturers’ literature and among clinicians, that ‘three dimensions’ (i. They ascribed this finding to the introduction of improved films and film-screen combinations. While these factors undoubtedly contributed to a lowering of doses, the situation is somewhat more complex. With intraoral radiology, there has been a shift over the past 20 years by manufacturers from low operating potentials (50 kVp or less) to higher operating potentials (65–70 kVp) and constant potential equipment. In parallel, there has been a shift from round to rectangular collimation of the X ray beam. The long working lifespan of dental X ray equipment means that the changes do not occur overnight, but emerge gradually as old equipment is phased out. It is important to remember, however, that these changes in equipment may not yet have had an impact in many countries, where there is evidence of continuing use of older, higher dose, equipment [19–21]. Even in the wealthiest countries, there is sometimes a reluctance to adopt even low (or zero) net economic cost methods of optimization, such as faster film speeds [22]. For panoramic radiography, analagous improvements in equipment design have contributed to lower individual patient doses, notably through field size limitation. Digital technology offers the potential of lowering patient doses, although the wide exposure latitude of digital systems, along with the absence of medical physics support, means that there is a risk of dentists not taking advantage of such opportunities. Matching the field of view to the diagnostic task permits significant dose reductions to be achieved, not least by taking organs of importance (e. While manufacturers seem to be responding to calls for improvements in these deficiencies, it is likely that existing equipment will continue in clinical use for many years. Working in isolation means that dentists can become inured to sub-optimal quality. The growing use of digital imaging has had a positive impact by removing chemical processing, deficiencies of which are a common cause of poor image quality. As pointed out above, ‘real world’ radiation doses from dental diagnostic X ray examinations often do not reflect those quoted in the scientific literature. In the United Kingdom, for example, dental reference doses have been reduced over the years since their introduction [23], suggesting that when dentists are alerted to a possibility of lowering dose to patients they respond positively to external advice. In many countries, however, there are no widespread dose audits of dental X ray equipment and no mechanism of facilitating optimization of exposures. Nonetheless, the large number of examinations, the high paediatric use, the primary care location, inconsistent or complete lack of interaction with medical physics support, self-referral and the long working lifespan of dental X ray equipment all suggest that complacency is not appropriate. First, education in radiation protection must be part of the undergraduate dental curriculum and reinforced through lifelong learning.
Practitioners are too busy with clinical and administrative work quality 20mg paroxetine; ongoing professional development and teaching methodology may not be optimal for adult education discount paroxetine 10mg with amex. Some referrers do not appreciate the difference in the use of medical imaging between community and tertiary settings. The challenges for guidance tools to facilitate the lowering of exposure in radiography, fluoroscopy and mammography are access to them, and the ways they are presented. The workforce shortage is global and is compounded by inequitable distribution, migration and changing practice models, e. In others, while magnetic resonance imaging is available and more appropriate, its use is limited by criteria to contain cost. The resources available to accurately monitor and record patient dose in radiography, fluoroscopy and mammography vary greatly. It is becoming challenging for some authorities to implement timely policy updates. For the end users, teleradiology threatens communication and disrupts team efforts in justification, optimization, error reduction, quality assurance, the control of repeats, the audits of doses and image quality, and the use of diagnostic reference levels, etc. For actions involving many stakeholders, there is a risk of poor coordination or fragmentation. Without good communication and collaboration, duplication and unintended complication are possibilities. Personnel and leadership changes could lead to discontinuity of long term actions. Ineffective advocacy, poor awareness and inadequate peer support are threats to volunteering. Radiation protection actions compete with other projects for funding, thus joint resource mobilization is more effective. Many system based actions have a long lead-time and it is important to persevere, stay focused and maintain motivation with these long term plans. The first is a framework of measures, strategies and process improvements for health care systems and end users [3]. The three measures are justification, optimization and error minimization, which are used along the patient journey. For the realization of any action, it is important to narrow the gaps between knowledge and practice. Each step of an action requires the contribution from different stakeholders who play unique roles. Effective advocacy improves the probability of policy adoption and use by practitioners. Under this radiation protection framework, a range of implementation strategies is used. Research includes conducting population exposure surveys and procedure exposure in facilities. The strengthening of advocacy, awareness, training, workforce capacity, physical infrastructure, policies, evaluation and ongoing improvement apply to health care systems and end users. There is synergy between these strategies and collectively they add value to each other. The common vehicles supporting these actions are evidence based recommendations and tools. Keeping these tools current; matching the contents to the setting; improving their user friendliness, format, media and search function; and securing end user support will lead to better acceptance and use. All actions are interrelated and synergy should be sought to maximize the outcome. Based on the findings of population and procedure exposure surveys, improvement actions should follow. Similarly laboratory developed quality control measures should be integrated into daily practice when appropriate. One of the issues limiting the development and implementation of these actions is the availability of human and financial resources. To maximize resources and synergy, and to minimize duplication, collaboration under an integrated framework is useful. A global platform such as this forum, the International Action Plan for the Radiological Protection of Patients [4], the International Basic Safety Standards [5], the World Health Organization’s Global Initiative on Radiation Safety in Healthcare Settings [6] and the global referral guidelines project [7] facilitate leader and stakeholder engagement across disciplines and sectors, communication, collaboration, team building, innovation, development of a safety culture and resource mobilization. Using a framework such as the one discussed, together with good teamwork, will overcome many of the emerging challenges and narrow the gaps between evidence and practice. These actions will improve patient care through doing the right procedure (justified) and doing the procedure right (optimized and without error), each time. Most principles for dose reduction in screen-film radiography, including justification, are relevant to digital systems. Paroxetine
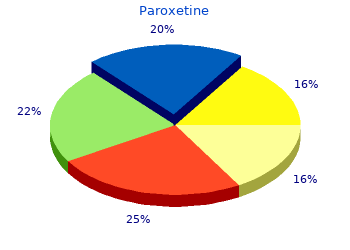
10 of 10 - Review by U. Aidan Votes: 84 votes Total customer reviews: 84 |
|